Upfront on Healthcare: Blog
At Upfront, we care deeply about the future of healthcare. We’re bringing you the most relevant and cutting-edge perspectives to help make that future a reality.

Blog
 Carrie Kozlowski, COO & Co-Founder
Carrie Kozlowski, COO & Co-Founder
Upfront hosts two-day user conference for Urgent Care industry leaders
 Carrie Kozlowski, COO & Co-Founder
Carrie Kozlowski, COO & Co-Founder
Upfront recently hosted a two-day user conference with Urgent Care leaders in Chicago. Leaders discussed challenges facing the industry, exchanged lessons from the field, and shared the strategies they’re applying to build a strong future. Read on as Upfront co-founder and COO, Carrie Kozlowski, shares her personal highlights from the event. https://vimeo.com/859826518 Last week, we […]

Blog
 Lindsay Zimmerman, PhD, MPH, Vice President, Bartosch Patient Activation Institute
Lindsay Zimmerman, PhD, MPH, Vice President, Bartosch Patient Activation Institute
What healthcare gets wrong about patient engagement (Hint: Sending a text message isn’t enough.)
 Lindsay Zimmerman, PhD, MPH, Vice President, Bartosch Patient Activation Institute
Lindsay Zimmerman, PhD, MPH, Vice President, Bartosch Patient Activation Institute
Sending mass text messages and simply crossing our fingers that patients will follow through with visits isn’t enough to win their trust or stand against the competition. So, how can healthcare enterprises earn patient loyalty? There is no silver bullet, and it certainly isn’t going to work until advanced personalization, a skill companies such as Amazon have already mastered, becomes a top strategic priority across the entire organization.
Blog
 Carrie Kozlowski, COO & Co-Founder
Carrie Kozlowski, COO & Co-Founder
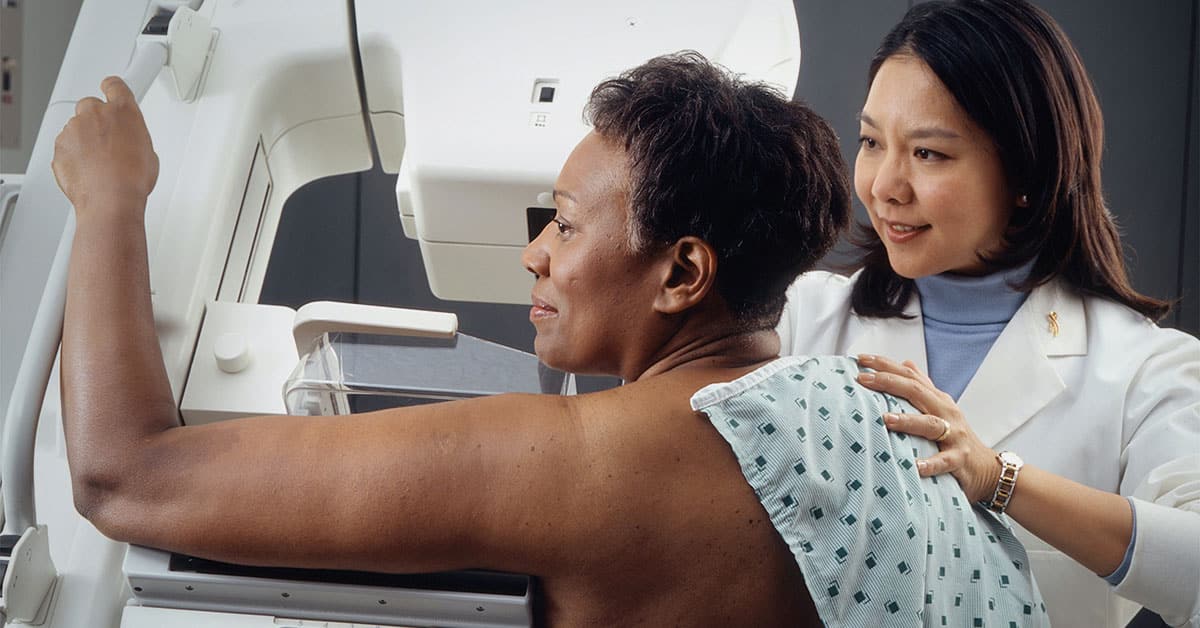
Now that breast cancer screenings have been dialed back to age 40, healthcare enterprises must plan ahead to tackle emerging care gaps
 Carrie Kozlowski, COO & Co-Founder
Carrie Kozlowski, COO & Co-Founder
As if patients’ slow return to care following the pandemic wasn’t a challenging premise enough, healthcare enterprises now face an emerging care gap — in breast health. Last week, the U.S. Preventive Services Task Force issued new draft guidelines about preventative care, effectively dropping the age of recommended breast cancer screening to a decade earlier, from the age of 50 to just 40 years.

Blog
 Upfront Healthcare, Staff
Upfront Healthcare, Staff
The spotlight is on … Shanika Gracien, Data Analyst
 Upfront Healthcare, Staff
Upfront Healthcare, Staff
Helping people has always been in Shanika Gracien’s DNA. So, it wasn’t a surprise that the daughter of Haitian immigrants would choose to follow an enviable path into healthcare. But after studying to become a physician’s assistant in college, and interning for various clinics and hospitals, Shanika encountered one, slight problem: “I realized I didn’t like the sight of blood,” she laughs. Here’s how Shanika pivoted her career journey to combine her love for helping others with a role in tech to advance patient health from behind the scenes, as a Data Analyst at Upfront.

Blog
 Brent Walker, Senior Vice President, Psychographics
Brent Walker, Senior Vice President, Psychographics
5 Effective Hospital Patient Loyalty Programs to Know
 Brent Walker, Senior Vice President, Psychographics
Brent Walker, Senior Vice President, Psychographics
Loyalty programs are common in most of the business world, but they are relatively new within the field of healthcare. However, as the need to boost patient loyalty increases, more hospitals are exploring the idea of implementing hospital patient loyalty programs in their institutions. Benefits of Patient Loyalty Programs Patient loyalty programs offer several benefits […]

Blog
 Brent Walker, Senior Vice President, Psychographics
Brent Walker, Senior Vice President, Psychographics
3 Practical Examples of Psychographic Segmentation in Marketing
 Brent Walker, Senior Vice President, Psychographics
Brent Walker, Senior Vice President, Psychographics
In today’s digitally-driven economy, it’s a common practice for marketers and advertisers of all kinds to collect data about the consumers and prospects who interact with their brand. Today’s well-informed consumer also understands this fact, and as a result, they generally expect a higher level of engagement with the companies whose products or services they […]